Bawul na huhu

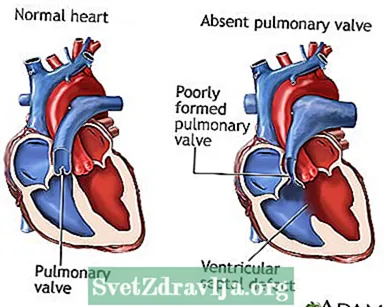
Bawul na huhu wani lahani ne wanda a ciki bawul na huhu ya ɓace ko kuma an kafa shi da kyau. Jini mara kyau na oxygen yana gudana ta wannan bawul daga zuciya zuwa huhu, inda yake karbar sabon iskar oxygen. Wannan yanayin yana nan yayin haihuwa (na haihuwa).
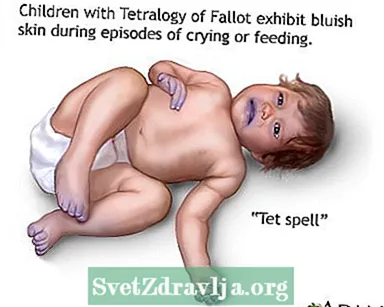
Bawul na huhu na faruwa lokacin da bawul na huhu bai samu ba ko ya inganta yadda ya kamata yayin da jaririn ke cikin mahaifar uwar. Idan ana ciki, yakan faru ne a matsayin wani ɓangare na yanayin zuciya da ake kira tetralogy na Fallot. An samo shi a cikin kusan 3% zuwa 6% na mutanen da suke da tetralogy na Fallot.

Lokacin da bawul na huhu ya ɓace ko baya aiki da kyau, jini baya gudana da kyau zuwa huhu don samun isashshen oxygen.
A mafi yawan lokuta, akwai rami ma tsakanin hagu da dama na zuciya (ƙwararrakin ƙugu na huɗu). Wannan nakasa kuma zai haifar da fitar da isashshen jini a jiki.
Fatar za ta sami bayyanar shuɗi (cyanosis), saboda jinin jiki yana ƙunshe da ƙarancin oxygen.
Bawul na huhu kuma yana haifar da kara girma (fadada) jijiyoyin huhu na huhu (jijiyoyin da suke daukar jini zuwa huhu don ɗaukar iskar oxygen). Zasu iya fadada sosai har su danna kan bututun da ke kawo iskar oxygen cikin huhu (bronchi). Wannan yana haifar da matsalar numfashi.
Sauran lahani na zuciya waɗanda zasu iya faruwa tare da bawul na huhu sun haɗa da:
- Valvearfin tricuspid mara kyau
- Defectunƙarar raunin atrial
- Outofar madaidaiciya madaidaiciya biyu
- Ductus arteriosis
- Launin matashi na Endocardial
- Ciwon Marfan
- Tricuspid atresia
- Rashin hawan jijiyoyin hagu
Matsalar zuciya da ke faruwa tare da bawul na huhu na iya zama saboda lahani a wasu ƙwayoyin halitta.
Kwayar cutar na iya bambanta dangane da waɗancan lahani da jariri ke da shi, amma na iya haɗawa da:
- Launin launin shuɗi zuwa fata (cyanosis)
- Tari
- Rashin cin nasara
- Rashin cin abinci
- Saurin numfashi
- Rashin numfashi
- Hanzari
Ana iya bincikar bawul na huhu kafin a haifi jariri da gwajin da ke amfani da igiyar ruwa don ƙirƙirar hoton zuciya (echocardiogram).
Yayin gwaji, mai ba da kiwon lafiya na iya jin gunaguni a cikin kirjin jariri.
Gwaje-gwaje don bawul na huhu sun haɗa da:
- Gwaji don auna aikin lantarki na zuciya (electrocardiogram)
- Zuciyar CT
- Kirjin x-ray
- Echocardiogram
- Hanyoyin fuska ta maganadisu (MRI) na zuciya
Yaran da ke da alamun numfashi galibi suna buƙatar tiyata nan da nan. Yaran da ba su da alamun bayyanar cututtuka galibi ana yin tiyata a tsakanin watanni 3 zuwa 6 na farkon rayuwarsu.
Dogaro da nau'in sauran lahani na zuciya da jariri yake dashi, tiyata na iya ƙunsar:
- Rufe ramin a bangon tsakanin hagu da hagu na zuciya na zuciya (nakasar raunin ciki)
- Rufe bututun jini wanda ya hada aorta da jijiyar huhu (ductus arteriosis)
- Ara fadada daga dama zuwa huhun
Nau'ukan tiyata don bawul na huhu sun haɗa da:
- Matsar da jijiyar huhu zuwa gaban aorta kuma nesa da hanyoyin iska
- Sake ginin bangon jijiyar cikin huhu don rage matsin lamba akan hanyoyin iska (kwayar cutar huhu da rage arterioplasty)
- Sake ginin bututun iska da numfashi zuwa huhu
- Sauya bawul na huhu mara kyau tare da ɗayan daga jikin mutum ko na dabba
Yaran da ke da alamun bayyanar numfashi mai tsanani na iya buƙatar samun iskar oxygen ko kuma a sanya su a kan na’urar numfashi (iska) kafin da bayan tiyata.
Ba tare da tiyata ba, yawancin jariran da ke fama da cutar huhu za su mutu.
A lokuta da yawa, tiyata na iya magance yanayin kuma yana taimakawa bayyanar cututtuka. Sakamakon yana da kyau sosai.
Matsaloli na iya haɗawa da:
- Ciwon kwakwalwa (ƙurji)
- Rushewar huhu (atelectasis)
- Namoniya
- Dama-gefe zuciya ta kasa
- Buguwa
Kirawo mai ba ka sabis idan jaririnku na da alamun bazuwar huhu na huhu. Idan kuna da tarihin iyali na lahani na zuciya, kuyi magana da mai ba ku kafin ko yayin cikin.
Kodayake babu wata hanyar da za ta hana wannan yanayin, ana iya kimanta iyalai don sanin haɗarinsu ga lahani na haihuwa.
Rashin ciwon bawul na huhu; Rashin haihuwa na bawul na huhu; Phenmonary bawul agenesis; Cyanotic cututtukan zuciya - bawul na huhu; Cutar cututtukan zuciya - bawul na huhu; Zuciyar haifuwa - bawul na huhu
 Bawul na huhu
Bawul na huhu Cyanotic 'Tet sihiri'
Cyanotic 'Tet sihiri' Tetralogy na Fallot
Tetralogy na Fallot
Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM. Acyanotic cututtukan cututtukan zuciya: raunin regurgitant. A cikin: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Littafin koyar da ilimin yara. 21st ed. Philadelphia, PA: Elsevier; 2020: babi na 455.
Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM. Raunukan cututtukan zuciya na Cyanotic: raunuka da ke haɗuwa da ragin jini na huhu. A cikin: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Littafin koyar da ilimin yara. 21st ed. Philadelphia, PA: Elsevier; 2020: babi na 457.
Scholz T, Yin tunani BE. Cutar cututtukan zuciya. A cikin: Gleason CA, Juul SE, eds. Cututtukan Avery na Jariri. 10 ed. Philadelphia, PA: Elsevier; 2018: babi na 55.
Webb GD, Smallhorn JF, Therrien J, Redington AN. Cutar cututtukan ciki a cikin baligi da haƙuri na yara. A cikin: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald na Ciwon Zuciya: Littafin rubutu na Magungunan zuciya da jijiyoyin jini. 11th ed. Philadelphia, PA: Elsevier; 2019: babi na 75.
