Ciwon mara

Ankylosing spondylitis (AS) wani nau'i ne na cututtukan zuciya. Yawanci yana shafar ƙasusuwa da haɗin gwiwa a gindin kashin baya inda yake haɗuwa da ƙashin ƙugu. Waɗannan haɗin gwiwa na iya zama kumbura da kumburi. Bayan lokaci, kashin kashin baya da ya shafa na iya haɗuwa.
AS shine babban memba na dangi mai kamanni na cututtukan zuciya da ake kira spondyloarthritis. Sauran membobin sun hada da cututtukan zuciya na psoriatic, amosanin gabbai na cututtukan hanji da cututtukan zuciya. Dangin amosanin gabbai ya zama na kowa kuma yana shafar mutum 1 cikin 100.
Ba a san dalilin AS ba. Halittu kamar suna taka rawa. Yawancin mutane tare da AS suna da tabbaci ga kwayar HLA-B27.
Cutar ta kan fara ne tsakanin shekaru 20 zuwa 40, amma tana iya farawa kafin shekara ta 10. Yana kamuwa da maza fiye da mata.
AS yana farawa da ƙananan ciwon baya wanda yake zuwa da baya. Painananan ciwon baya yana kasancewa a mafi yawan lokuta yayin da yanayin ke ci gaba.
- Jin zafi da taurin rai sun fi muni da daddare, da safe, ko lokacin da ba ku da ƙarfi. Rashin jin daɗi na iya tashe ka daga barci.
- Ciwon yakan zama mafi sauƙi tare da aiki ko motsa jiki.
- Ciwon baya na iya farawa a tsakanin ƙashin ƙugu da kashin baya (sacroiliac joints). Bayan lokaci, yana iya ƙunsar duka ko ɓangaren kashin baya.
- Spineananan kashin baya na iya zama mara sassauƙa. Bayan lokaci, ƙila za ku iya tsayawa a gaban gaba.
Sauran sassan jikinka da ka iya shafar sun hada da:
- Haɗuwa na kafadu, gwiwoyi da ƙafafun kafa, waɗanda na iya kumbura da zafi
- Abubuwan haɗin tsakanin haƙarƙarinku da ƙashin ƙirjinku, don haka ba za ku iya faɗaɗa kirjinku sosai ba
- Ido, wanda yana iya samun kumburi da ja
Gajiya kuma alama ce ta gama gari.
Ananan alamun bayyanar sun haɗa da:
- Zazzaɓi kaɗan
AS na iya faruwa tare da wasu yanayi, kamar:
- Psoriasis
- Ciwan ulcer ko cutar Crohn
- Sake dawowa ko kumburin ido (iritis)
Gwaje-gwaje na iya haɗawa da:
- CBC
- ESR (ma'aunin kumburi)
- HLA-B27 antigen (wanda ke gano kwayar halittar da ke da alaƙa da ankylosing spondylitis)
- Rheumatoid factor (wanda ya kamata ya zama mummunan)
- X-ray na kashin baya da ƙashin ƙugu
- MRI na kashin baya da ƙashin ƙugu
Mai ba da sabis na kiwon lafiya na iya ba da umarnin magunguna irin su NSAIDs don rage kumburi da ciwo.
- Wasu NSAIDs ana iya siyan kan-kan-kan (OTC). Wadannan sun hada da aspirin, ibuprofen (Advil, Motrin), da naproxen (Aleve, Naprosyn).
- Sauran NSAIDs an tsara su ta mai ba da sabis.
- Yi magana da mai baka ko likitan harka kafin amfani da dogon lokaci na kowane NSAID.
Hakanan zaka iya buƙatar magunguna masu ƙarfi don sarrafa ciwo da kumburi, kamar:
- Corticosteroid far (kamar prednisone) da aka yi amfani da shi na ɗan gajeren lokaci
- Sulfasalazine
- Masanin ilimin halitta na TNF-kamar su etanercept, adalimumab, infliximab, certolizumab ko golimumab
- Mai hana ilimin ilimin halitta na IL17A, secukinumab
Yin aikin tiyata, kamar maye gurbin hanji, ana iya yi idan ciwo ko haɗin gwaiwa ya yi tsanani.
Motsa jiki zai iya taimakawa inganta yanayin aiki da numfashi. Kwanciya kwance a bayanku da daddare zai iya taimaka muku kiyaye yanayin yadda kuke.
Halin cutar yana da wuyar faɗi. Bayan lokaci, alamu da alamun bayyanar AS flareup (sake dawowa) da nutsuwa (gafara). Yawancin mutane suna iya yin aiki da kyau sai dai idan suna da lahani sosai a kwatangwalo ko kashin baya. Kasancewa cikin ƙungiyar tallafi na wasu masu matsala iri ɗaya na iya taimakawa sau da yawa.
Jiyya tare da NSAIDS yakan rage zafi da kumburi. Jiyya tare da masu hanawa na TNF da wuri a cikin cutar ya bayyana ne don rage saurin ciwan kashin baya.
Ba da daɗewa ba, mutanen da ke fama da cutar sankarau na iya samun matsala tare da:
- Psoriasis, rashin lafiyar fata na kullum
- Kumburi a cikin ido (iritis)
- Kumburi a cikin hanji (colitis)
- Bugun zuciya mara kyau
- Ararƙasawa ko kuma ɗaura ƙwayoyin huhu
- Tsanyawa ko kaurin bawul na zuciya
- Lalacewar laka bayan faɗuwa
Kira mai ba da sabis idan:
- Kuna da alamun cututtukan cututtukan zuciya
- Kuna da cututtukan cututtuka da ke haifar da sababbin bayyanar cututtuka yayin jiyya
Spondylitis; Spondyloarthritis; HLA - Spondylitis
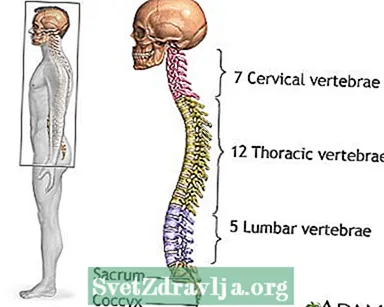
 Kwayar kasusuwa
Kwayar kasusuwa Ciwon mahaifa
Ciwon mahaifa
Gardocki RJ, Park AL. Rashin nakasawa na thoracic da lumbar spine. A cikin: Azar FM, Beaty JH, Canale ST, eds. Bellungiyar Orthopedics ta Campbell. 13th ed. Philadelphia, PA: Elsevier; 2017: babi na 39.
Inman RD. Abubuwan da ke amfani da su. A cikin: Goldman L, Schafer AI, eds. Magungunan Goldman-Cecil. 26th ed. Philadelphia, PA: Elsevier; 2020: babi na 249.
van der Linden S, Brown M, Gensler LS, Kenna T, Maksymowych WP, Taylor WJ. Ankylosing spondylitis da sauran siffofin axial spondyloarthritis. A cikin: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelly's Littafin rubutu na Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021: babi na 80.
Ward MM, Deodhar A, Gensler LS, et al. Sabuntawa na 2019 na Kwalejin Kwalejin Rheumatology na Amurka / Spondylitis Association of America / Spondyloarthritis Bincike da Hanyar Sadarwar Sadarwa Shawarwarin don maganin cututtukan cututtukan zuciya da nonradiographic axial spondyloarthritis. Arthritis Kulawa Res (Hoboken). 2019; 71 (10): 1285-1299. PMID: 31436026 pubmed.ncbi.nlm.nih.gov/31436026/.
Werner BC, Feuchtbaum E, Shen FH, Samartzis D. Ankylosing spondylitis na kashin baya na mahaifa. A cikin: Shen FH, Samartzis D, Fessler RG, eds. Littafin rubutu na Cervical Spine. Philadelphia, PA: Elsevier Saunders; 2015: babi na 28.
